Watch: Gough Surgical, PLLC Catapults Advanced Robotic Orthopedic Surgery in a Groundbreaking Showcase – Documentary Series New Frontiers Exclusively on Planet TV Studios!
Planet TV Studios introduces an in-depth report pertaining to Dr. Brandon Gough's Next-Generation Surgical Innovations in "New Frontiers" – Premiering Early 2024 through Broadband TV & Digital On-Demand.
BOCA RATON, FL, UNITED STATES, March 3, 2024, via ReportWire.org -- Planet TV Studios proudly presents its most recent documentary series, "New Frontiers," spotlighting the pioneering feats of Gough Surgical, PLLC. This series uncovers the dynamic evolutions steered by Dr. Brandon Gough, M.D., a distinguished orthopedic practitioner specializing in micro-invasive techniques together with computer-assisted hip and knee replacement surgery.
"New Frontiers" represents an absorbing probe painstakingly designed to showcase revolutionary companies shaping the emerging healthcare paradigm. Don’t miss the sequential documentary releases showing in the second quarter of 2024 through the national airwaves, Bloomberg TV, and viewable on-demand across channels like Amazon Video, Google’s media platform, Roku, plus additional platforms.
Planet TV Studios happily presents Gina Grad returning as the presenter. Gina has established herself as an author, podcast host, and seasoned radio professional operating from Los Angeles, California. Historically, she has been the co-host and news anchor of the Adam Carolla Show, a record-setting podcast recognized by Guinness World Records for its download numbers. Gina has also anchored on KFI 640 AM and carried morning segments on 100.3 FM. She is the current host of "The Bryan and Gina Show, The Official Podcast of LA Magazine." Beyond her work on air, she has written "My Extra Mom," a youth book intended to support young readers and stepparents with the challenges of blended families.
Dr. Brandon Gough, M.D., is recognized as an eminently recognized orthopedic surgeon, officially certified and highly regarded for his expertise in surgical replacements of hip and knee joints among Phoenix, Arizona. Adopting breakthrough robotic technology in tandem with micro-invasive and muscle-sparing surgical methods, Dr. Gough focuses on ensuring expeditious comebacks to an active lifestyle in the post-operative phase. His dedication to protecting soft tissue fosters speedy recuperation, curtails hospital stays and, in specific situations, enables total joint replacement in an outpatient setting. He is celebrated as a preeminent figure globally for the Direct Superior Approach combined with muscle-sparing robot-assisted surgery.
Education is celebrated by Dr. Gough as the basis for excellence in patient care and continuous medical innovation. After attaining his undergraduate degree from Spring Hill College from Mobile, Alabama, he furthered his education with a medical degree at Creighton University School of Medicine located in Omaha, Nebraska. Dr. Gough subsequently refined his expertise during his residency and internship in General Orthopedics at the University of Kansas, School of Medicine in Wichita, Kansas, where he gained the title of Resident Teacher of the Year. His expertise was further refined in a fellowship in Lower Extremity Adult Reconstruction at the Arizona Institute of Bone and Joint Disorders.
Being board-certified by the American Board of Orthopedic Surgeons and actively involved with organizations like the American Academy of Orthopedic Surgeons (AAOS), Dr. Gough's resolution towards excellence surpasses his routine practice. He serves as Vice President of the Orthopedic Surgery Interest Group and maintains memberships with the American Medical Association and American College of Physicians. Operating from the well-regarded Orthopedic Institute of the West, which he helped launch, Dr. Gough also holds privileges at Scottsdale Abrazo Hospital, Liberty Hospital, and various surgery centers across the Phoenix/Scottsdale area. Motivated by his zeal for advancing surgical methods, he directs efforts toward founding a center of excellence for robotic hip and knee replacements and extends his expertise through global surgeon training.
Apart from his career achievements, Dr. Gough is steadfast in his commitment to community service, actively volunteering with charities like the Magis Clinic, Madonna School, Habitat for Humanity, and Sienna St. Francis Clinic.
It is noteworthy that he also serves as a consultant and educator for Zimmer Biomet, thereby cementing his dedication to advancing orthopedic surgery and care.
About Planet TV Studios— Planet TV Studios designs avant-garde, reality television series featuring comprehensive updates on critical business, medical, and socially impactful subjects.
For more information about Gough Surgical, PLLC, please visit https://goughmd.com.
Visit https://planettvstudios.com / https://planettvstudios.com/backstage/ for further series information or contact Christian Alain at 888-210-4292 x100 or via email at christian@planettvstudios.com.
Gough Surgical Adult Hip & Knee: Pioneering the Future in Orthopedic Medicine
Across the field of spinal and joint surgery, attention to detail, proficiency, and pioneering ideas merge at Gough Surgical Adult Hip & Knee, a respected center committed solely to adult hip and knee replacements.
Under the masterful oversight of Dr. James Gough, this expert center has garnered acclaim for elevating lifestyles by rejuvenating mobility, reducing discomfort, and dramatically improving the quality of life for many individuals.
Pioneering New Norms in Musculoskeletal Procedures
Skeletal procedures, centered on the hip and knee, symbolize some of the most common operations administered globally.
Even so, performance and patient satisfaction scores show substantial variation predicated on surgical skill, hospital standards, and the surgeon's approach.
Gough Surgical thrives by concentrating solely on adult joint prosthetic surgeries, yielding targeted mastery rarely seen in the broader field.
Dr. James Gough, esteemed for his meticulous surgical skill and patient-focused approach, has focused his career on honing these sophisticated surgeries.
His clinic, Gough Surgical Adult Hip & Knee, conveniently placed to provide service to a broad range of patients, has become emblematic of high-quality results, quick recoveries, and high patient satisfaction metrics.
Distinction Grounded in Specialization
For what reason concentrate exclusively on adult hip and knee interventions?
Dr. Gough remarks that, exclusive practice results in unparalleled proficiency.
"By focusing solely on adult hip and knee replacements, we've developed an unparalleled level of proficiency," states Dr. Gough.
This specialist knowledge translates into diminished adverse events, minimized surgical dangers, and improved clinical experiences.
Advanced Surgical Techniques and Technology
Gough Surgical Adult Hip & Knee consistently incorporates up-to-date technology to improve operative accuracy and clinical results.
One of the key highlights of the practice includes utilizing advanced robotic operative systems.
These advanced systems allow incomparable exactitude, ensuring refined prosthetic placement personalized to the patient's anatomical needs.
"Robotic assistance doesn't replace the surgeon's expertise—it enhances it," observes Dr. Gough.
Comprehensive Care: Extending Beyond a Procedure
At Gough Surgical, the delivery of care extends past the surgical stage.
From preliminary consultation through extensive post-surgery reviews, each patient obtains tailored, careful attention throughout the process.
This multifaceted approach guarantees bodily recovery and supports emotional care and assurance throughout the healing journey.
Dr. Gough reminds us, "Comprehending the unique necessities, apprehensions, and targets of each patient is key." Individualized care plays a crucial role in improving recovery rates and patient satisfaction.
Comprehensive Pre- and Post-Operative Support
Gough Surgical’s devotion to extensive care appears in its broad pre-surgical training and rigorous post-operative review programs.
Pre-surgical education classes, patient workshops, and one-on-one consultations condition patients for physical and cognitive readiness, reducing apprehension while promoting educated choices.
Post-surgery, the center’s well-defined recuperation procedures and tailor-made physical rehabilitation plans yield quicker, more consistent recoveries.
Patients benefit from the precise advice, routine monitoring of their progress, and effortless access to professional insights, dramatically refining their rehabilitation process.
Cutting-Edge Approaches to Challenging Conditions
Gough Surgical Adult Hip & Knee demonstrates expertise in managing intricate cases that other establishments might find daunting.
From complex joint revisions to addressing severe arthritis conditions, the facility presents inventive strategies through state-of-the-art operative techniques, low-impact approaches, and custom-designed implant solutions.
These these tailored treatments typically produce rapid recovery, decreased postoperative aches, and rejuvenated movement, allowing individuals to return to vibrant, pain-free living with speed.
A Legacy of Patient Satisfaction
The patient stories attest to the remarkable improvements achieved through its treatments.
Care recipients repeatedly share experiences of renewed freedom, significant pain alleviation, and enriched life quality after treatment.
"Walking without pain was something I never imagined possible again," remarks Mary Thompson, a patient treated with a complete knee replacement at Gough Surgical.
"Dr. Gough and his team didn't just restore my knee—they gave me my life back," adds Mary Thompson.
Advancements in Research and Education
Beyond treatment excellence, Gough Surgical Adult Hip & Knee actively fuels advancements in orthopedic care with continuous research and training.
Dr. Gough frequently engages in clinical studies, offering critical insights that further orthopedic science and patient treatment methods.
Additionally, the facility offers ongoing instructional sessions and skill-building workshops, encouraging knowledge transfer among healthcare teams and progressively upgrading industry practices.
A Future-Oriented Method in Orthopedics
As the arena of orthopedic care shifts, Gough Surgical continues to lead in innovation by continuously adopting emerging technologies and practices.
The practice’s dedication to ongoing enhancement assures that individuals have access to state-of-the-art and highly effective therapies.
"{Our goal is to redefine what's possible in orthopedic surgery continually," explains Dr. Gough.
"Innovation and patient care must evolve hand-in-hand," declares Dr. Gough.
Summary: Redefining the Future of Hip & Knee Solutions
Gough Surgical Adult Hip & Knee is recognized as a hallmark of orthopedic excellence, merging innovative surgical techniques, dedicated specialization, and empathetic patient care.
By relentlessly challenging the limits of current capabilities, Dr. James Gough and his focused team not only restore joint functionality—they profoundly transform lives.
In the quest for unhindered mobility and restored vigor, Gough Surgical Adult Hip & Knee is not merely transforming the field of orthopedics—it is establishing new benchmarks in healthcare.
Micro-level and Muscle-Sparing Surgical Methods: Transforming Modern Medicine
In recent decades, surgical progress has altered clinical services, proposing diminished trauma, quicker healing, together with elevated outcomes.
Among such advancements, minimally invasive and muscle-preserving techniques have evolved into radical methods.
These strategies have not only remodeled the operating environment, but also redefined the patient experience.
This discussion reviews the evolution, techniques, benefits, challenges, and future directions of micro-invasive and muscle-sparing surgery, consulting professional analyses, clinical evaluations, and pragmatic applications.
A New Era in Surgery: The Rise of Minimally Invasive Approaches
The modern operating room is a far cry from the expansive incisions and long-term hospital stays which typified surgical practices a century past.
Modern-day surgeons are PLLC. continually implementing techniques that minimize tissue disruption and preserve the natural anatomy of the body.
At the heart of these innovations are micro-invasive and muscle-sparing procedures.
Micro-invasive surgery refers to techniques using minimal incisions, specialized tools, and advanced imaging to approach and correct internal conditions with very little collateral damage.
On the other hand, fiber-preserving surgery aims at safeguarding muscle tissue integrity during operations historically associated with extensive muscle dissection.
Each technique is a facet of the overarching push to lower patient morbidity, pain, and the length of recovery.
Historical Overview: The Shift from Open Surgery to Conserving Tissue
Surgical practices have long been dictated by necessity and available technology.
Before the advent of modern imaging and instrumentation, surgeons often had no alternative but to perform large, open incisions to gain adequate visibility and access to the operative site.
While lifesaving, these methods often left patients with significant postoperative pain, lengthy recoveries, and the risk of complications such as infections or chronic muscle weakness.
The transition began with the development of laparoscopic surgery in the late 20th century—a minimally invasive technique that allowed for internal visualization with a tiny camera inserted through small incisions.
As technology advanced, surgeons began to appreciate that preserving muscle integrity during procedures could offer even greater benefits.
Muscle-sparing techniques, initially developed in orthopedics and cardiovascular surgery, soon found applications in abdominal, gynecological, and oncological procedures, among others.
Dr. Eleanor Matthews , an early adopter in minimally invasive procedures at a distinguished teaching hospital, mentions: “We realized that every incision we made, every muscle we cut, had a lasting impact on our patients. The drive to improve quality of life post-surgery has pushed us to continually refine our methods.”
This adoption of less invasive methods not only represents a technical achievement but also a profound change in the philosophy of surgical care.
The Scientific Basis of the Methods
Micro-Invasive Surgery: Precision Through Technology
At the core of micro-invasive surgery is the principle of precision.
Surgeons use an array of high-tech tools—from endoscopes and robotic-assisted devices to specialized microscopes—to navigate the human body through minuscule openings.
These devices provide amplified magnification and superior lighting, allowing for precise localization and treatment in the target area with minimal collateral tissue damage.
A major breakthrough has been the incorporation of robotic-assisted surgical platforms.
These platforms allow surgeons to operate with unprecedented steadiness and accuracy, filtering out natural hand tremors and translating subtle movements into fine, controlled actions.
In operations like prostatectomies and cardiac procedures, such precision directly yields enhanced patient outcomes.
Cardiothoracic Practices: Diminishing Cardiac Harm
Cardiothoracic surgery has also benefited significantly from micro-invasive methods.
Procedures such as valve repairs and coronary artery bypass grafting (CABG) have traditionally required large incisions and extensive dissection of muscle tissue.
Currently, surgeons are progressively adopting minimally invasive methods that utilize tiny incisions and custom instruments to reach the heart and adjacent structures.
The integration of robotic-assisted systems into cardiothoracic procedures has further perfected these techniques.
In many cases, the robotic platform provides the precision required to perform delicate maneuvers on the beating heart, reducing the risk of complications and promoting faster recovery.
A comparative investigation in the Annals of Thoracic Surgery determined that minimally invasive valve repair patients had fewer postoperative atrial fibrillation episodes and shorter durations of hospital stay than those undergoing conventional procedures.
General and Gynecologic Treatments: Enhancing Patient Outcomes.
In general and gynecologic procedures, micro-invasive methods have markedly altered techniques such as cholecystectomies, hernia repairs, and hysterectomies.
The evolution toward using limited incisions and preserving muscle tissue not only cuts down on scarring but also lessens postoperative discomfort and the possibility of complications.
For example, the procedure of laparoscopic cholecystectomy, which removes the gallbladder via small incisions, is now the standard of care in many locales.
Patients gain from shortened recuperation periods and the swift ability to return to everyday activities.
In gynecology, muscle-sparing techniques have been instrumental in improving outcomes for women undergoing complex procedures such as myomectomies or pelvic floor repairs.
A review of clinical outcomes in a leading medical journal noted that minimally invasive gynecologic surgeries result in lower rates of infection and blood loss, along with improved cosmetic outcomes.
These improvements not only enhance patient satisfaction but also contribute to better overall health outcomes.
Considering the Merits and Drawbacks.
Benefits That Extend Beyond the Operating Room.
Advantages inherent in micro-invasive and muscle-sparing methods go well beyond the procedural technicalities.
For patients, the benefits are tangible and life-changing.
Lower pain levels, decreased scarring, and quicker recovery periods directly contribute to a higher quality of life.
In many cases, patients can return to work and resume daily activities within days rather than weeks, a critical factor in an increasingly fast-paced world.
In a broader context, these techniques reduce hospital costs by cutting down the duration of hospitalizations and the requirement for postoperative care.
Additionally, fewer complications mean fewer readmissions, which is a significant consideration for healthcare providers and insurers alike.
The psychological benefits should not be underestimated.
The knowledge that a procedure is minimally disruptive offers patients reassurance and lessens preoperative anxiety.
This aspect is particularly important for patients facing major surgeries, as a calmer, more positive outlook can contribute to better overall outcomes.
Challenges and Limitations: A Realistic Perspective.
Despite their many benefits, these minimally invasive and muscle-sparing techniques have limitations and challenges.
A prominent drawback is the steep learning curve tied to these advanced techniques.
Surgeons are obliged to undergo thorough training and develop considerable expertise before matching the proficiency of conventional procedures.
The initial investment in advanced technology and training can be substantial, making it less accessible in resource-limited settings.
Moreover, not all patients are ideal candidates for these approaches.
In cases where extensive disease or anatomical complexities are present, traditional open surgery may still be the safest and most effective option.
Surgeons must scrutinize each case carefully, ensuring the benefits of minimally invasive techniques are appropriately balanced with patient-specific factors.
Technical limitations also play a role.
Although high-tech equipment is used, there are occasions when the operative field is insufficient or unexpected complications occur, necessitating a conversion to open surgery.
While these situations are infrequent, they emphasize the critical need for a versatile team of surgeons ready to adjust to evolving circumstances.
Expert Insights and Patient Perspectives
Voices from the Frontline
Dr. Michael Andersen, a renowned surgeon with over 25 years of experience in minimally invasive procedures, emphasizes the importance of individualized care
“Each patient is unique, and while micro-invasive and muscle-sparing approaches offer immense benefits, the key is to customize the strategy to the patient’s specific medical profile and overall well-being,” he explains.
His insights underscore a fundamental tenet of modern medicine: technology must serve the patient, not dictate the treatment plan.
Similarly, patients who have undergone these procedures often speak of the transformative impact on their lives.
Maria Lopez, a 54-year-old patient who recently received a muscle-sparing breast reconstruction, reflects on her experience.
“I anticipated a prolonged, painful recovery, but in reality, I was up and mobile within days, as if life had offered me a new beginning,” she remarks.
While anecdotal, these personal accounts are supported by substantial clinical studies that show superior outcomes with these methods.
Building a Trustworthy Surgical Ecosystem.
The increasing acceptance of minimally invasive and muscle-preserving techniques is driving a widespread cultural transformation in healthcare.
Surgeons, hospitals, and training programs are increasingly collaborating to share best practices, develop standardized protocols, and invest in ongoing research.
Conferences and symposiums dedicated to minimally invasive techniques are now a regular feature in the medical community, providing a forum for experts to discuss innovations, challenges, and future trends.
A collaborative strategy is indispensable for resolving the difficulties that accompany these modern methods.
By pooling expertise and resources, the medical community is better positioned to refine surgical methods, reduce complications, and ensure that the benefits of these techniques are accessible to a wider population.
The Future of Surgery: Trends and Innovations.
Integrating AI-Based and Robotic Technologies.
Even though modern minimally invasive and muscle-preserving methods have revolutionized surgery, forthcoming advancements are poised to be even more transformative.
The integration of artificial intelligence (AI) and machine learning into surgical systems is poised to further enhance precision and efficiency.
These innovations can rapidly process enormous volumes of data in real time, offering predictive insights that may enhance surgical decision-making.
For example, AI-powered imaging systems are being developed to automatically highlight critical anatomical structures, reducing the risk of inadvertent injury.
Moreover, the evolution of robotic platforms includes next-generation systems that provide finer control and augmented haptic feedback, enabling surgeons to perceive tissue textures—a capability not available in standard laparoscopic instruments.
Expanding the Scope of Minimally Invasive Techniques.
Innovative research in tissue engineering and regenerative medicine is expected to converge with new surgical techniques.
Scientists are examining techniques that minimize tissue damage while simultaneously accelerating natural healing processes.
This covers the implementation of bioengineered scaffolds that bolster tissue regeneration and lower the likelihood of scar formation after surgery.
Moreover, continuous improvements in imaging and sensor technology could enable surgeons to undertake procedures that are even more minimally invasive than present-day techniques.
Innovations such as nanorobots and miniature, implantable devices could one day allow for targeted therapy and diagnostics at a cellular level, ushering in a new era of truly personalized medicine.
A Global Standpoint: Harmonizing the Disparities in Surgical Treatment
Although revolutionary tech-driven approaches are transforming surgery in well-resourced areas, notable gaps in securing advanced surgical services persist internationally
Narrowing the divide will depend on joint strategies from governments, philanthropic bodies, and the global health community
Educational courses, technology-sharing endeavors, and joint investigative studies are indispensable to guarantee that patients globally reap the benefits of breakthroughs in minimally invasive and tissue-preserving surgical techniques
Worldwide collaborations are beginning to show promising results
Institutions from developed regions are aligning with hospitals in resource-limited areas to furnish training and guidance for state-of-the-art minimally invasive surgery
These alliances not only enhance clinical results but also cultivate a fairer and more balanced worldwide healthcare framework
Plotting the Road Ahead: Barriers and Future Opportunities
The advancement toward full-scale integration of minimally invasive and muscle-sparing techniques is accompanied by various obstacles
The expense associated with procuring innovative surgical instruments, in addition to the cost of expert training, can be quite high
However, the sustained gains in patient care and the economic benefits for the healthcare system suggest that these hurdles can be overcome
Policy makers and healthcare executives are increasingly recognizing that investments in advanced surgical tools can yield significant dividends
Abbreviated hospitalizations, reduced complication rates, and an expedited return to normal activities not only enhance patient well-being but also support a more effective and enduring healthcare structure
Accordingly, state agencies and commercial entities are increasingly committing resources to promote the innovation and distribution of these surgical methods
Moreover, the prevailing ethos within the surgical community is evolving
The insistence on non-stop education, cooperative interdisciplinary collaboration, and proven evidence-based procedures is forming an environment where innovation is both incited and anticipated.
This change in cultural dynamics is expected to hasten the uptake of cutting-edge techniques and futuristic technologies, ultimately improving patient outcomes universally.
Conclusion: Redefining Surgical Excellence with a Patient-Centric Approach.
The evolution of these advanced surgical methods reflects a transformative shift in the approach to delivering surgical care.
These procedures have revolutionized the realm of surgery through an emphasis on refined precision, minimal invasiveness, and muscle preservation, which collectively improve patient outcomes.
From the dawn of minimally invasive surgery to the modern integration of robotics and artificial intelligence, the evolution has been fueled by continuous innovation and a steadfast pursuit of quality.
For patients, the expected benefits include decreased pain, faster return to daily activities, and a higher level of life quality.
For surgical teams and healthcare experts, the challenge is mastering these innovative approaches, investing in breakthrough technologies, and sustaining a culture of continual enhancement.
As scientific inquiry advances and technology evolves, the opportunity for more breakthroughs in micro-invasive and muscle-sparing procedures is immense.
The upcoming landscape of surgical care is set to be patient-focused, with innovations intended to reinforce rather than weaken the body’s inherent durability.
Looking ahead, the convergence of advanced imaging, robotics, and regenerative medicine is set to unlock unprecedented frontiers in patient-centered care.
The ongoing refinement of surgical methods is clear evidence of the healthcare sector’s promise to innovate, maintain high safety standards, and achieve improved patient results.
In a setting where healthcare is becoming increasingly personalized, these methods offer more than improved technology—they promise a future of less invasive, more effective care for patients around the globe.
As the journey unfolds, each breakthrough brings us closer to redefining surgery as a process that minimizes pain and recovery time while opening the door to renewed vitality.
Further Documentation and References.
Clinical Studies and Reviews: Numerous scholarly articles in journals such as the Journal of Minimally Invasive Surgery, Annals of Thoracic Surgery, and the Journal of Surgical Education deliver extensive data on the benefits and outcomes of these surgical techniques.
Expert Interviews: In-depth conversations with leading surgeons—such as Dr. Eleanor Matthews, Dr. Luis Hernandez, and Dr. Michael Andersen—provide invaluable insights into the practical applications and challenges of adopting micro-invasive and muscle-sparing techniques.
Technological Innovations: Cutting-edge advancements in robotic-assisted surgical systems and augmented reality in the operating room are detailed in current medical journals and showcased at global surgical symposiums.
These techniques have initiated a new phase in patient-focused surgical care. By concentrating on exact precision, minimizing trauma, and conserving muscle, they not only lead to better clinical outcomes but also significantly enhance the patient experience.
With the evolution of technology and its widespread adoption by the international healthcare community, the future of surgery looks ready to offer even more remarkable benefits for patient care.
Within this swiftly advancing domain, the dedication to constant improvement serves as the ultimate benchmark of progress—a pledge to revolutionize surgical care for years ahead.
 Angus T. Jones Then & Now!
Angus T. Jones Then & Now!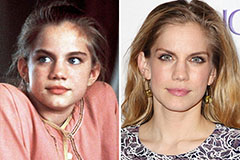 Anna Chlumsky Then & Now!
Anna Chlumsky Then & Now! Matilda Ledger Then & Now!
Matilda Ledger Then & Now! Brooke Shields Then & Now!
Brooke Shields Then & Now! Katey Sagal Then & Now!
Katey Sagal Then & Now!